USMLE Reviewer
(By Subscription)
The skeletal and muscular shell of the thorax encloses the heart and lungs, powers breathing, and is the mechanical platform for arm and neck motion.
It is bounded anteriorly by the sternum and ribs, laterally and posteriorly by the ribs, and supported posteriorly by the spine.
The inferior boundary is the diaphragm and rib margins. Superiorly, it is bounded by the clavicles and soft tissues of the neck. The thoracic wall includes the bodies of the 12 thoracic vertebrae, the 12 pairs of ribs, and the sternum.
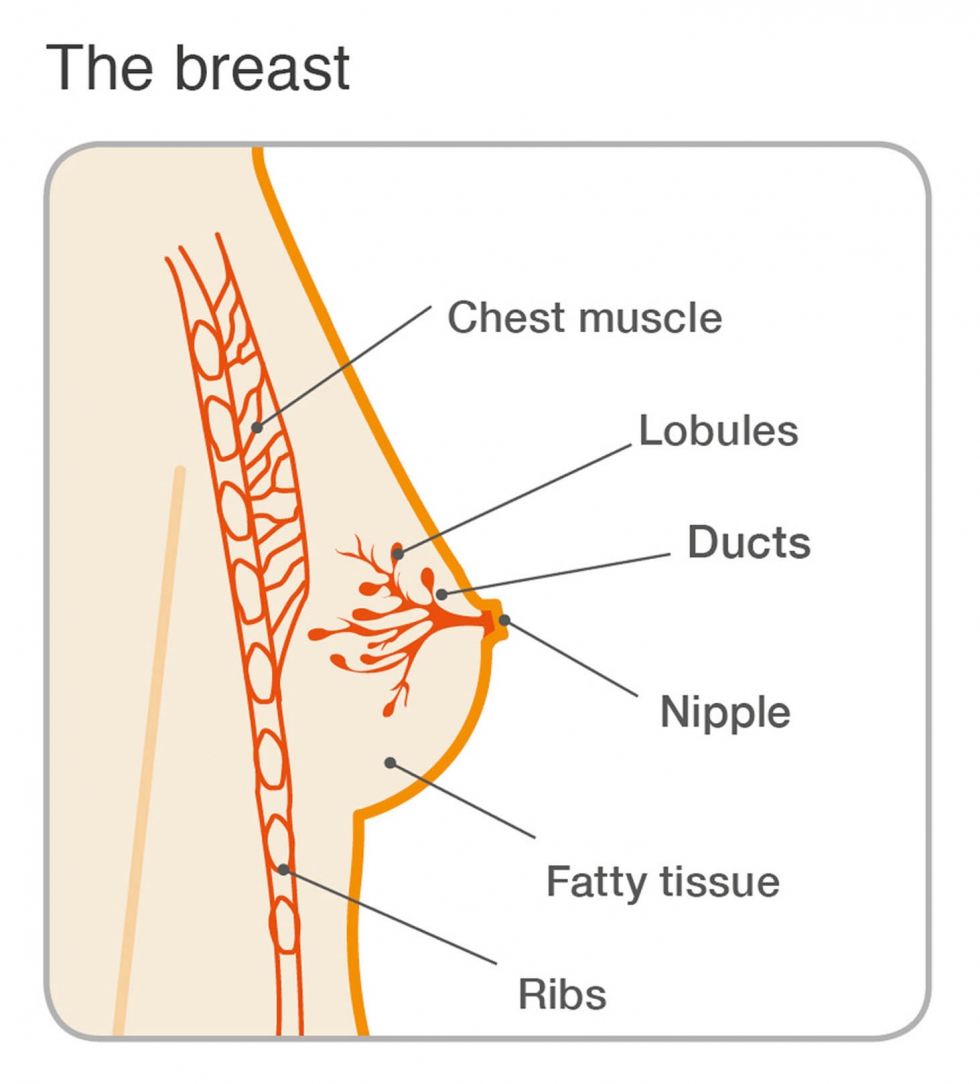
The female breast consists of subcutaneous, radially arranged, mammary gland tissue and fat, typically extending from ribs 2 through 6 superiorly to inferiorly and from the sternal border to the midaxillary line.
The mammary gland is a subcutaneous structure located within the superficial fascia.
The breast is anterior the deep fascia related to the pectoralis major and serratus anterior muscles. The retromammary space is a layer of loose connective tissue that separates the breast from the deep pectoral fascia.
The breast overlies the pectoralis major and the anterior portion of the serratus anterior muscles. A portion of breast tissue extends into the axilla as the axillary tail of Spence.
The tail of Spence is a triangular tongue-shaped portion of breast tissue that extends superiorly and laterally toward the axilla, perforating the deep axillary fascia, and enters the axilla, where it terminates in close proximity to the axillary lymph nodes and vessels as well as the axillary blood vessels and nerves.
For descriptive purposes, the breast divided into quadrants. Each breast is centered by the elevated nipple, which contains the openings of the lactiferous ducts and is composed of circular smooth muscle. Surrounding the nipple is pigmented skin or the areola, which contains the opening of the lubricating sebaceous glands. The radially arranged mammary gland tissue forms 15 to 20 lobes, each drained by a lactiferous duct that has a dilatation called the lactiferous sinus just before its opening onto the nipple. The lobes are irregularly separated by incomplete dense connective tissue septae that attach to the dermis of the overlying skin. These septae, called the suspensory ligaments (of Cooper), are especially well developed in the superior half of the breast.
The breast is supplied by branches of the internal thoracic, lateral thoracic, and anterior and posterior intercostal arteries. The breast is innervated by anterior and lateral cutaneous branches of intercostal nerves.
+++++++++++++++
The long thoracic nerve lies close to the midaxillary line.

Saggital section of the breast. (Reproduced, with permission, from Lindner HH. Clinical Anatomy. East Norwalk, CT: Appleton & Lange, 1989:202.)
Lymphatic drainage of the breast begins as a subareolar plexus. The majority of lymph drained from the breast (usually quantified at 75%) drains to the axillary lymph nodes. The axillary node group is often described as a pyramid, like the axilla, and is typically subdivided into five subgroups: pectoral (anterior), lateral (humeral), posterior (subscapular), central (medial), and apical. Lymph from the axillary nodes typically drains into the inferior deep cervical lymph nodes. However, lymph from the axillary node group may drain into other nodes such as the interpectoral and deltopectoral nodes (Figure 26-2). This is especially true in instances of metastasis because “normal” paths become blocked by the malignancy and alternate routes must be established. The pectoral, humeral, and subscapular nodes are level 1 nodes, whereas the central and apical nodes are level 2 and 3 nodes, respectively.
The medial quadrants of the breast will have lymph drain into the parasternal lymph nodes along the internal thoracic vessels. Some lymph from the inferior quadrants may drain to inferior phrenic nodes.

Lymphatics of the breast. (Reproduced, with permission, from Lindner HH. Clinical Anatomy. East Norwalk, CT: Appleton & Lange, 1989:205.)
2. Be able to list the primary path for lymphatic drainage of the breast and the several subgroups of the axillary nodes.
3. Be able to describe the secondary pathways for lymph drainage.
The long thoracic nerve lies close to the midaxillary line. For descriptive purposes, it is divided into quadrants. Each breast is centered by the elevated nipple, which contains the openings of the lactiferous ducts and is composed of circular smooth muscle. Surrounding the nipple is pigmented skin or the areola, which contains the opening of the lubricating sebaceous glands. The radially arranged mammary gland tissue forms 15 to 20 lobes, each drained by a lactiferous duct that has a dilatation called the lactiferous sinus just before its opening onto the nipple. The lobes are irregularly separated by incomplete dense connective tissue septae that attach to the dermis of the overlying skin. These septae, called the suspensory ligaments (of Cooper), are especially well developed in the superior half of the breast. A loose connective tissue layer, the retromammary space, separates the breast components and the pectoral fascia, allowing for some movement. The breast overlies the pectoralis major and the anterior portion of the serratus anterior muscles. A portion of breast tissue typically extends into the axilla as the axillary tail (of Spence). The breast is supplied by branches of the internal thoracic, lateral thoracic, and anterior and posterior intercostal arteries. The breast is innervated by anterior and lateral cutaneous branches of intercostal nerves.
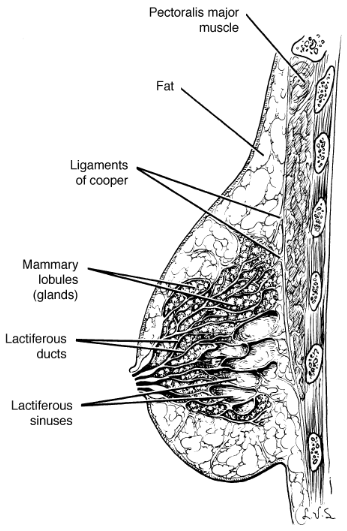
Saggital section of the breast. (Reproduced, with permission, from Lindner HH. Clinical Anatomy. East Norwalk, CT: Appleton & Lange, 1989:202.)
Mammary Gland Structure
Each gland consists of 15 to 20 radially aligned lobes of glandular tissue. A lactiferous duct drains each lobe (Figure A and B). The lactiferous ducts converge and open onto the nipple. The nipple is positioned on the anterior surface of the breast and is surrounded by a somewhat circular hyperpigmented region, the areola. Sebaceous glands within the areola enlarge to form swollen tubercles during pregnancy as the areola darkens. Small collections of smooth muscle located at the base of the nipple may cause erection of the nipple when breast feeding or sexually aroused.

A. Anterior view of the breast. B. Sagittal section of the breast. C. Arterial supply of the breast. D. Lymphatic drainage of the breast.
Fibrous and adipose tissues occupy the spaces between the lobes of glandular tissue. To help support the weight of the breast, strong fibrous bards called suspensory (Cooper's) ligaments separate the lobes and attach between the dermis and deep layer of the superficial fascia.
Arteries, Veins, and Lymphatics of the Breast
To simplify an understanding of vascular supply and lymphatic drainage, the breast's anatomy can be best understood by division into medial and lateral regions (Figure C and D).
Medial region of the breast. Derives its blood supply from perforating branches of the internal thoracic artery (medial mammary branches from the second through fourth intercostal spaces) and is drained by internal thoracic veins. Lymphatic vessels exiting the medial side of the breast drain into the parasternal lymph nodes, which lie beside the internal thoracic veins.
Lateral region of the breast. Derives its blood supply from branches of the lateral thoracic artery (axillary artery origin) and mammary branches from the 2nd through the 5th posterior intercostal arteries (thoracic aorta origin) and is drained by the lateral thoracic and intercostal veins, respectively. The lymphatic vessels draining the lateral side of the breast lead primarily into the pectoral group of axillary lymph nodes and account for most of the lymph drained from the breast. Figure D shows lymph from the right breast draining into the right lymphatic duct at the junction of the right brachiocephalic vein. In contrast, the left breast (not shown) drains into the thoracic lymphatic duct at the left brachiocephalic vein junction.
Some breast lymphatics drain into the infraclavicular group of axillary nodes, as well as the supraclavicular group of deep cervical nodes.
Breast augmentation is a procedure that is performed to enhance the shape and size of the breast. The procedure is frequently performed for cosmetic reasons or for breast reconstruction. The implant (filled with saline or silicone) may be inserted from various incision sites. Regardless of the incision site, the implant is placed in one of two areas, either subglandular (between the pectoralis major muscle and the mammary gland) or submuscular (deep to the pectoralis major muscle).
Most breast adenocarcinomas are lactiferous duct carcinomas that begin as painless masses, most commonly in the upper lateral quadrant.
Innervation of the Breast
The sensory innervation of the skin overlying the breast has a segmental arrangement and is supplied by branches of the 2nd through 7th intercostal nerves. However, physiologic changes in the breast are not mediated by nerves but by circulating hormones. For example, high prolactin levels result in milk production, and oxytocin causes the milk “letdown” reflex.
The breast receives its principal blood supply from perforating branches of the internal mammary artery, lateral branches of the posterior intercostal arteries, and branches from the axillary artery, including the highest thoracic, lateral thoracic, and pectoral branches of the thoracoacromial artery.
The majority of lymph drained from the breast (usually quantified at 75%) drains to the axillary lymph nodes. The rest flows through the lymph vessels that accompany the perforating branches of the internal mammary artery and enters the parasternal (internal mammary) group of lymph nodes.
Lymphatic drainage of the breast begins as a subareolar plexus. The axillary node group is often described as a pyramid, like the axilla, and is typically subdivided into five subgroups: pectoral (anterior), lateral (humeral), posterior (subscapular), central (medial), and apical. Lymph from the axillary nodes typically drains into the inferior deep cervical lymph nodes. However, lymph from the axillary node group may drain into other nodes such as the interpectoral and deltopectoral nodes (Figure 26-2). This is especially true in instances of metastasis because “normal” paths become blocked by the malignancy and alternate routes must be established. The pectoral, humeral, and subscapular nodes are level 1 nodes, whereas the central and apical nodes are level 2 and 3 nodes, respectively.
The medial quadrants of the breast will have lymph drain into the parasternal lymph nodes along the internal thoracic vessels. Some lymph from the inferior quadrants may drain to inferior phrenic nodes.

Lymphatics of the breast.
Muscles of the Anterior Thoracic Wall
These muscles also function as accessory respiratory muscles by helping to expand the thoracic cavity when inspiration is deep and forceful.
Muscle |
Proximal Attachment |
Distal Attachment |
Action |
Innervation |
|---|---|---|---|---|
Pectoralis major |
Clavicle, sternum, and costal rib margins |
Lateral intertubercular groove of humerus |
Flexion, adduction, medial rotation of humerus |
Medial (C8–T1) and lateral (C5–C7) pectoral nn. |
Pectoralis minor |
Attaches anteriorly on the thoracic skeleton to ribs 3 to 5 |
Superiorly to the coracoid process of the scapula. |
Protraction and stabilization of scapula against the thoracic wall. |
Medial pectoral n. (C8–T1) |
Serratus anterior |
Lateral border of ribs 1–8 Attaches to ribs 1 to 8 along the midaxillary line and courses posteriorly to the medial margin of the scapula. The serratus anterior muscle is a primary protractor of the scapula as well as a stabilizer of the scapula against the thoracic wall. |
Medial margin of scapula |
Protraction and stabilization of scapula |
Long thoracic n. (C5–C7) |
Subclavius |
Rib 1 |
Clavicle |
Stabilize clavicle |
Nerve to subclavius (C5–C6) |

A. Muscles of the anterior thoracic wall. B. Intercostal muscles. Note the step dissection showing the intercostal muscles. C. Axial illustration of the intercostal muscle group.
The area between ribs is the intercostal space (Figure 2-3B and C).

A. Muscles of the anterior thoracic wall. B. Intercostal muscles. Note the step dissection showing the intercostal muscles. C. Axial illustration of the intercostal muscle group.
The eleven intercostal spaces each contain three overlapping layers of tissue consisting of the external, internal, and innermost intercostal muscles and membranes. Intercostal nerves and vessels, coursing between the second and third layers of muscles (from superficial to deep), supply the intercostal muscles. The intercostal muscles are muscles of respiration and are named according to their positions to one another.
Study Question
During thoracocentesis, the needle is pushed in the intercostal space superior to the rib to prevent damage to the intercostal nerve, artery, and vein. Beginning with the external intercostal muscles and ending with the pleural space, which thoracic wall layers, from superficial to deep, does the needle penetrate?
Endothoracic fascia, internal intercostal muscles, costal parietal pleura, and pleural cavity
Internal intercostal muscles, innermost intercostal muscles, mediastinal parietal pleura, endothoracic fascia, and pleural cavity
Internal intercostal muscles, innermost intercostal muscles, costal parietal pleura, endothoracic fascia, and pleural cavity
Internal intercostal muscles, innermost intercostal muscles, endothoracic fascia, costal parietal pleura, and pleural cavity
E. Innermost intercostal muscles, internal intercostal muscles, endothoracic fascia, costal parietal pleura, and pleural cavity
The nerve and blood supply of the thoracic wall consists largely of the neurovascular elements that course through the intercostal spaces. The major elements in each space consist of an intercostal vein, artery, and nerve. The primary neurovascular bundle courses along the costal groove of the upper rib, between the internal and innermost intercostal muscles. The anterior and posterior intercostal arteries supply the intercostal spaces and form anastomoses with each other.
The intercostal nerves are derived from the ventral rami of the first 11 thoracic spinal nerves and are named accordingly (Figure 2-5A and B).

A. Axial section through the thorax showing the vascular supply. B. Intercostal structures. Schematic illustrating the thoracic veins (C) and the thoracic arteries (D).
For example, the right fifth intercostal nerve is derived from the ventral ramus of the fifth thoracic spinal nerve and courses through the right fifth intercostal space under the partial cover of the costal groove of the right fifth rib. The intercostal nerves give rise to the anterior and lateral cutaneous branches (sensory) and muscular branches (motor).
The thoracic wall receives its arterial supply from the following branches of the subclavian artery and thoracic aorta (Figure 2-5B and D):
 When the aortic arch is constricted (coarctated) just beyond the origin of the left subclavian artery, the anastomoses between the anterior and posterior intercostal arteries enable blood in the internal thoracic arteries to reach the descending aorta, bypassing the coarctation.
When the aortic arch is constricted (coarctated) just beyond the origin of the left subclavian artery, the anastomoses between the anterior and posterior intercostal arteries enable blood in the internal thoracic arteries to reach the descending aorta, bypassing the coarctation.
Venous drainage of the thoracic wall is from the following tributaries of the subclavian and azygos system of veins (Figure 2-5C):
Lymphatic drainage of the thoracic cavity is primarily through the following lymph nodes:
An intercostal artery is identified in a 44-year-old man who is undergoing thoracic surgery. This artery would most likely be located between which two structures?
The correct answer is D. You answered C.
The intercostal arteries and veins course between the internal and innermost intercostal muscles.
Content 2
Content 3
The thoracic skeleton consists of the thoracic vertebrae posteriorly, the ribs laterally, and the sternum and costal cartilages anteriorly. The costal cartilages secure the ribs to the sternum.
The thoracic cage forms a protective cage around vital organs such as the heart, lungs, and great blood vessels. The thoracic skeleton provides attachment points for the muscles of the back and chest that allow support of the shoulder girdle (scapula and clavicle) and movement of the upper limbs.
The 12 thoracic vertebrae articulate with the 12 pairs of ribs. Thoracic vertebrae typically bear two costal facets on each side, one at the superior edge and the other at the inferior edge of the vertebral body, where they receive the heads of the ribs (Figure 2-4A). The bodies of T10 to T12 vary from this pattern, however, by having only a single facet for their respective ribs. In addition, the T1 to T10 transverse processes have costal facets that articulate with the tubercles of the ribs.

A. Superior view of a thoracic vertebra articulating with ribs. B. Lateral and anterior views of the thoracic rib cage. C. Anterior and posterior views of a typical rib. D. Anterior view of the sternum.
Twelve pairs of ribs form the flared sides of the thoracic cage and generally extend anteriorly from the thoracic vertebrae to the sternum (Figure 2-4B). Rib pairs 1 to 7 are known as the true ribs and attach directly to the sternum by individual costal cartilages. The remaining five pairs of ribs are called false ribs because they either attach indirectly to the sternum or lack a sternal attachment entirely. Rib pairs 8 to 10 attach to the sternum indirectly by joining each other via costal cartilages immediately above. Rib pairs 11 and 12 are called floating ribs because they have no anterior attachments; instead, they are embedded in the muscles of the lateral body wall.
 Oblique course of ribs. The ribs course in an oblique, inferior direction from their thoracic vertebral articulation to their anterior sternal articulation. For example, rib 2 articulates with the T2 vertebra posteriorly but with the sternal angle at the T4 vertebral level anteriorly. Therefore, an axial section of the thorax, such as the one seen in a CT scan, intersects several ribs.
Oblique course of ribs. The ribs course in an oblique, inferior direction from their thoracic vertebral articulation to their anterior sternal articulation. For example, rib 2 articulates with the T2 vertebra posteriorly but with the sternal angle at the T4 vertebral level anteriorly. Therefore, an axial section of the thorax, such as the one seen in a CT scan, intersects several ribs.
Ribs 2 to 10 are considered typical ribs and have the following bony landmarks (Figure 2-4C):
 Fracture of a rib commonly occurs just anterior to the angle, the weakest point of the rib, and may puncture the parietal pleura, resulting in a pneumothorax.
Fracture of a rib commonly occurs just anterior to the angle, the weakest point of the rib, and may puncture the parietal pleura, resulting in a pneumothorax.
Ribs 1, 11, and 12 are atypical ribs. Rib 1 is not palpable because it lies deep to the clavicle. It has the scalene tubercle on the upper surface for the inferior attachment of the anterior scalene muscle. The groove for the subclavian vein is anterior to the scalene tubercle; the groove for the subclavian artery is posterior to the tubercle. Ribs 11 and 12 do not articulate with the sternum and receive the name “floating ribs.”
 The term “costal” means rib or rib-like part.
The term “costal” means rib or rib-like part.
The sternum, or breastbone, is flat and consists of the following structures (Figure 2-4D):
(By Subscription)